What Is Ovarian Stimulation?

Medically reviewed by Linda Streety, RN, BSN
The assisted reproductive technology in vitro fertilization (IVF) is a series of procedures that enable an egg and sperm to come together in a lab before being implanted in the uterus. The first part of this process is ovarian stimulation, during which the ovaries are stimulated with medications to produce multiple follicles (small sacs of fluid in which eggs grow). Once mature, eggs are retrieved from the follicles in a minor surgical procedure known as an “egg retrieval."
Below, we’ll walk you through the ovarian stimulation process, the types of medications used during ovarian stimulation, and how they will affect your body.

6 Second Snapshot
- During ovarian stimulation, your reproductive endocrinologist (RE) will prescribe a protocol of medications to encourage your body to develop more eggs than normal.
- When several follicles are roughly 17-18mm in diameter, your RE will schedule the trigger shot, which encourages your eggs to mature in preparation for retrieval.
- While ovarian stimulation can be a taxing process, there are steps you can take to prepare and manage symptoms.
What Happens During a Typical Menstrual Cycle?
At birth, ovaries already contain all the eggs they will ever grow! At puberty, the body begins to release these eggs during the menstrual cycle.
Ovulation occurs when the mature egg bursts from its follicle and travels down the fallopian tube, where it can be fertilized. If fertilization occurs, the resulting embryo attaches to the wall of the uterus. If fertilization does not occur within 12-24 hours of release from the ovary, the egg dissolves. Regardless of the length of your menstrual cycle, your period will occur about 12-14 days after you ovulate.
It may surprise you to know that eggs begin maturing three months before they are released. It may also surprise you to know that your body stimulates many follicles to grow eggs each month, but usually only releases one through ovulation.
What Happens During an Ovarian Stimulation Cycle?
During the fertility treatment known as ovarian stimulation, your reproductive endocrinologist (RE) will likely choose from one of four protocols. The timelines below should give you a general estimate of how long each protocol will take:
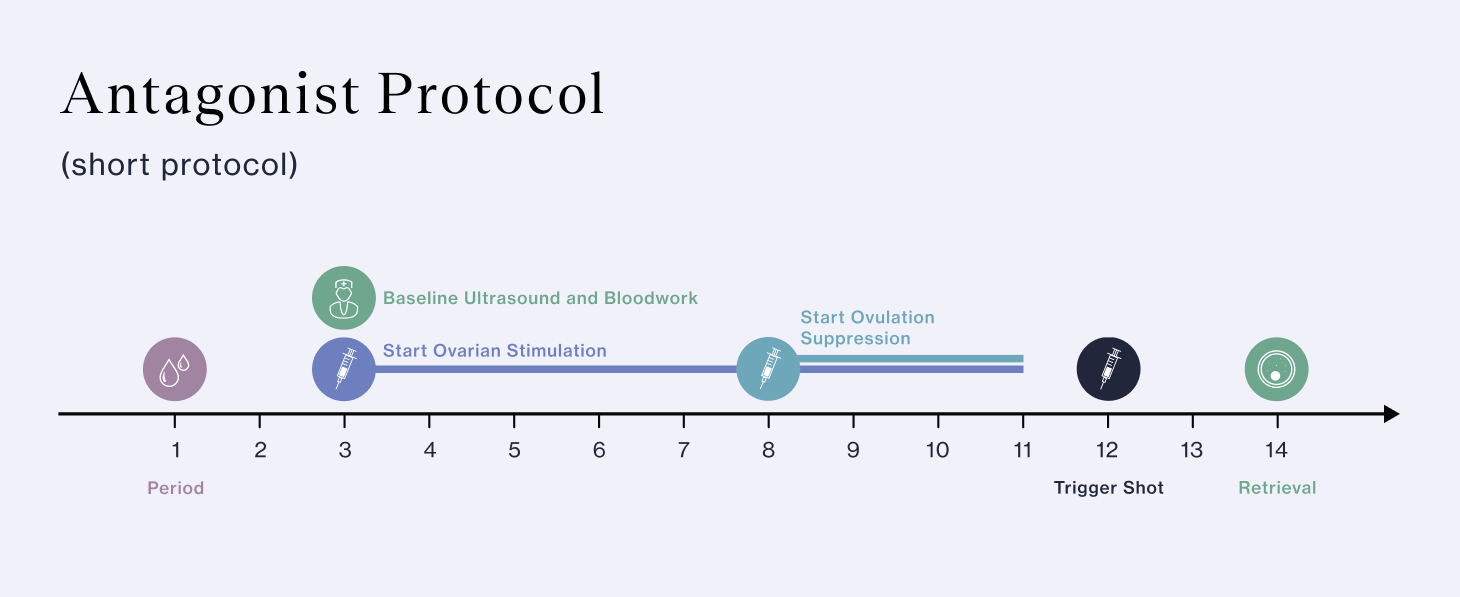
Antagonist protocol (short protocol): The most commonly used, this protocol begins with your menstrual cycle. This protocol lasts about 8-14 days and is better for patients at risk of ovarian hyperstimulation syndrome (OHSS). This protocol uses gonadotropins such as Follistim or Gonal-F and Menopur to stimulate the ovaries, ovulation suppression drugs such as Ganirelix or Cetrotide, and HCG or Lupron to trigger the eggs to mature for retrieval.
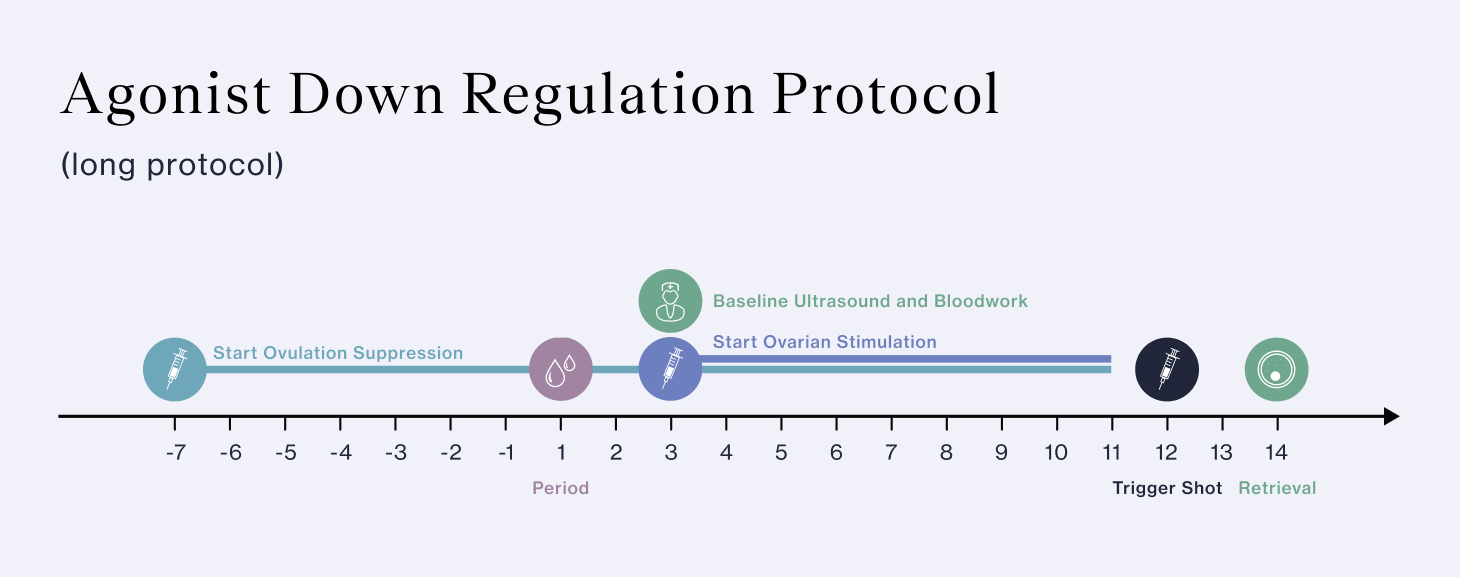
Agonist down regulation protocol (long protocol): This protocol uses medications to control your hormones before beginning ovarian stimulation. Since this protocol can take as many as 4-5 weeks, it requires more medications. Your RE may choose this protocol if you are at risk of premature ovulation. This protocol uses Lupron for ovulation suppression, Follistim or Gonal-F and Menopur to stimulate the ovaries, and HCG to trigger the eggs for retrieval.
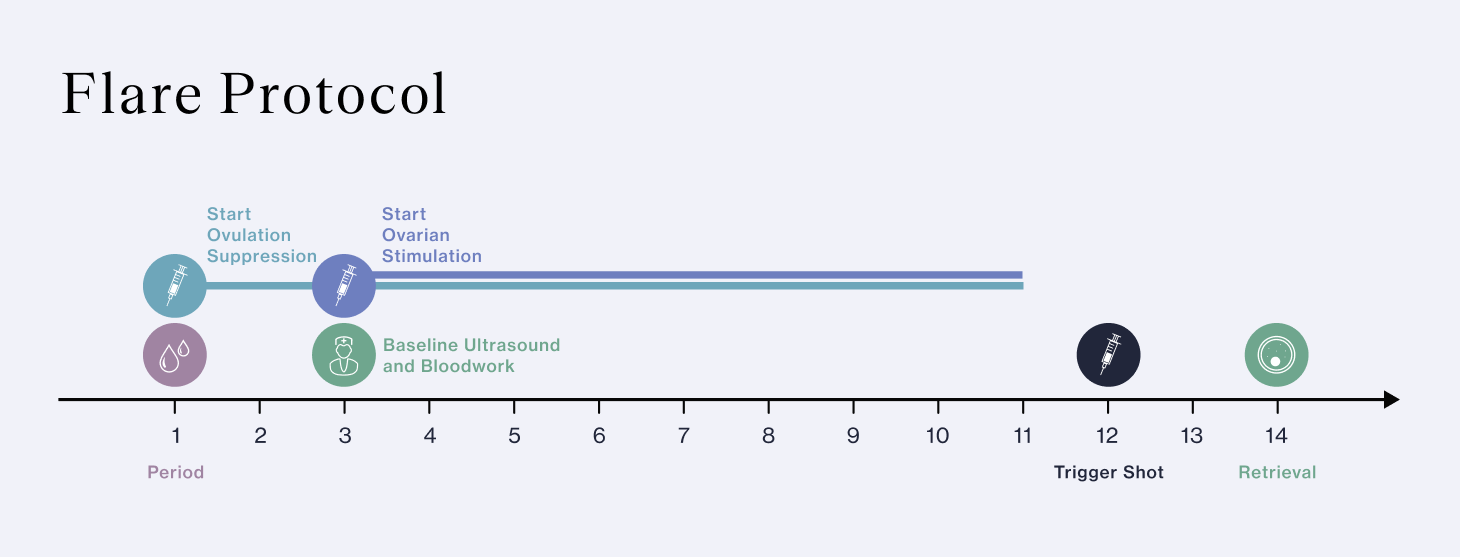
Flare protocol: The flare protocol encourages, rather than suppresses, production of FSH. The flare protocol is a good choice for patients who have responded poorly to other protocols, or who are of advanced maternal age. This protocol uses Lupron to suppress ovulation, Follistim or Gonal-F and Menopur to stimulate the ovaries, and HCG to trigger the eggs to mature for retrieval.
Mini-IVF: Minimal stimulation IVF or “mini-IVF” may be used if you have low ovarian reserve. Mini-IVF uses lower doses of stimulation medications and may involve oral instead of, or in conjunction, with injectable medications. Though mini-IVF is easier on your body, it usually results in just three to six eggs retrieved, lowering your chance of success.
Fertility medications for all four protocols have the same purpose: to encourage follicle growth, control the timing of ovulation, and retrieve up to 15-20 eggs. More than 20 eggs puts you at risk of OHSS, so your RE will manage your medications carefully to prevent that. Here is a breakdown of the process and the medications you may take to encourage more of your follicles to grow eggs to maturity while controlling ovulation. This ensures that your RE can retrieve as many mature eggs as possible.
This process starts with a fertility workup during the menstrual cycle before ovarian stimulation. Your RE will order blood tests to look at your levels of follicle-stimulating hormone (FSH), luteinizing hormone (LH), estradiol (E2), and anti-müllerian hormone (AMH). (To help you remember all of this new terminology, check out our cheat sheet of the top 12 IVF terms you need to know.) Your results will provide insight into your ovarian reserve (the remaining supply of eggs in your ovaries). Your RE will then decide on an ovarian stimulation protocol for you based on your personal goals and their findings.
Step 1: Preparing Ovaries for Stimulation
Depending on your baseline results, your RE may start you on medications before ovarian stimulation. These medications may include:
-
Birth control pills: These may help your ovaries respond to the stimulation medications, prevent ovarian cysts, and control the timing of your cycle.
-
Lupron (leuprolide acetate): A GnRH agonist, this medication prevents premature ovulation when taken before your cycle begins.
-
Estrace/estradiol valerate (estrogen): Your RE may start you on estrogen before your stimulation cycle to improve your ovarian response.
Step 2: Encouraging Follicle Growth
Each day, you will inject medications that encourage your follicles to develop eggs. The medications you may take include:
-
Gonal-F/Follistim (follitropin alfa): This gonadotropin drug contains recombinant follicle stimulating hormone (FSH), a hormone that occurs naturally in your body which encourages follicle growth.
-
Menopur (menotropins): This gonadotropin drug contains both FSH and luteinizing hormone (LH), both of which encourage follicle growth.
-
Clomid (clomiphene citrate): This drug stimulates the release of estrogen in the body, and can be used with other follicle stimulating drugs to encourage follicle growth.
Step 3: Maintaining Follicular Growth While Suppressing Ovulation
At a certain point during ovarian stimulation, your RE will add medications to prevent ovulation, which will give you the best chance of developing the optimal number of eggs without releasing them early. The medications your RE may add to your protocol include:
-
Lupron (leuprolide): During the down regulation protocol, Lupron is used to prevent premature ovulation.
-
Ganirelix/Cetrotide (ganirelix/cetrorelix): This medication prevents the LH surge that induces ovulation.
Step 4: Triggering Eggs to Mature For Retrieval
When several of your follicles have reached about 18-22mm in diameter (usually after 7-10 days), your doctor will schedule your trigger shot. This shot is carefully scheduled to occur 34-36 hours before egg retrieval to give your eggs a chance to mature. During maturation, your eggs will undergo meiosis, during which they will shed 23 out of their 46 chromosomes, allowing them to be potentially fertilized. Medications that trigger eggs to mature for retrieval include:
-
hCG: This medication contains human chorionic gonadotropin, which is very similar to LH, which triggers your eggs to mature.
-
Lupron (leuprolide): If you have not already taken Lupron to down-regulate you during your cycle, as with the antagonist protocol, it can be used to trigger your eggs to mature.
You’ve done it, your ovarian stimulation protocol is complete! You can now move on to the next important phase of the process, egg retrieval. You will be lightly sedated as your RE inserts an ultrasound-guided needle through your vaginal wall into each follicle to retrieve your eggs. Afterward, an embryologist will examine the eggs to determine how many were mature. At this point you may choose to either freeze your eggs or fertilize them with your partner’s or a donor’s sperm. After fertilization, your embryologist will prioritize which embryos are best suited for transfer to your uterus to complete the IVF process.
It is important to note that not all your eggs may be mature, and not all of your mature eggs may fertilize. At each step in the IVF process, some eggs or embryos do not make it to the next step. This is normal and expected, which is why your RE will try to optimize the number of eggs retrieved. The more eggs retrieved, the better your overall chance of success.
If you do not get as many mature eggs as you hoped during your ovarian stimulation process, it may help to know that patients tend to have more success during successive IVF cycles. This in part because your RE will use data from your ovarian stimulation cycle to better tailor your medication protocol on successive cycles. However, the data shows that even if you have the exact same medication protocol, you are likely to have a better outcome during your next cycle.
What Is The Ovarian Stimulation Process Like?
It’s time consuming! Many people are surprised by how much time and effort ovarian stimulation takes. During ovarian stimulation, you will need to go to the fertility clinic frequently for blood draws and transvaginal ultrasounds to check on your hormone levels and follicle growth. As you get close to the time for your trigger shot, you may have appointments every morning. This can require advance planning with work, childcare, and transportation.
Self-administering shots can be intimidating, but it can also be empowering. Undergoing ovarian stimulation is a way of taking control of your fertility, and many people feel empowered by the process. That said, there are things you can do to make the process smoother. The first is to understand how to administer the shots. There are many videos available online that walk you through the preparation of each medication, so you can take it step-by-step.
Ovarian stimulation shots are administered subcutaneously, so the needle is relatively short and often feels just like a pinch. It may help to change the spot where you administer the injections each day. You can numb your skin with an ice cube, or use a device such as the ShotBlocker or Buzzy to help reduce pain during the injection. You can also ask your partner, a friend, or family member to administer the shots for you.
Medication side effects can be challenging. Since ovarian stimulation medications are hormones that naturally occur in the body, they may produce side effects similar to what you experience during your menstrual cycle. So while you may have more energy during the follicular phase of your cycle when you have higher estrogen, you may experience tiredness, nausea, acne, weight gain, breast tenderness, and/or bloating after egg retrieval. You may also experience bloating and pain in your ovaries. If you are experiencing any of these symptoms, talk to your nurse or RE.
Rest matters. Ovarian stimulation is a time to get plenty of sleep and avoid high-impact exercise. You may also need a lot of rest after egg retrieval. Planning ahead to remove activities and stressors before you begin ovarian stimulation will help you have a successful cycle.
Avoiding Ovarian Hyperstimulation Syndrome (OHSS)
Ovarian Hyperstimulation Syndrome (OHSS) is an uncomfortable and potentially dangerous condition that may occur after egg retrieval if you developed a large number of follicles (more than 20) and/or had high estrogen levels before the trigger shot was administered. During OHSS, fluid builds up in the abdominal cavity. While OHSS was previously more common during IVF, the development of the antagonist protocol with a Lupron trigger has mostly eliminated this condition.
The symptoms of OHSS include bloating, constipation, reduced urinary output, and abdominal pain. If you suspect that you are experiencing OHSS, you should contact your clinic. However, if you notice that you are experiencing rapid weight gain (more than 2.2 pounds in one day), nausea and/or vomiting, severe abdominal pain, and/or shortness of breath, you should go to the emergency room for care.
To manage OHSS, your RE may recommend a high protein diet, plenty of electrolytes and fluids, and an over-the-counter stool softener.
Articles
Share this
Articles
Learn everything you need to know about IVF
Join the newsletter for IVF education, updates on new research, and early access to Alife products.